小黑娃把长长的美国胆囊疾病超声共识全文进行了整理归类,下面是精华部分18点:
1、胆囊息肉于体检超声检查中常被检出,又被称为胆囊息肉样病变,普通人群中发病率为3%~6%,大多数是良性的胆固醇性息肉或炎性息肉,但少部分可为肿瘤性息肉,具有恶变倾向。
2、研究结果表明,在直径>10 mm 的胆囊息肉中,仅有0.4%息肉癌变,且大多数恶性息肉通常测量值>20 mm。越来越多的证据显示绝大多数手术切除的胆囊息肉都是非肿瘤性息肉,因此,现阶段的胆囊息肉临床诊疗指南备受质疑。
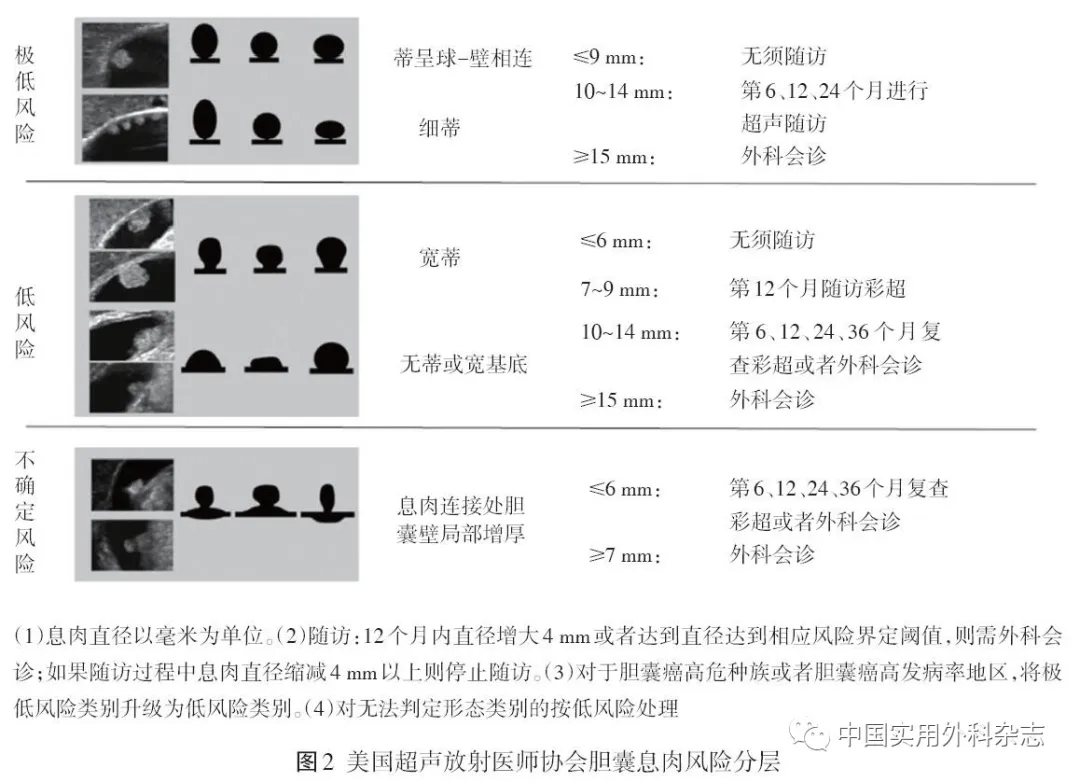
3、恶性息肉通常平均直径及生长速度要大于非恶性息肉,由此,共识建议在首次发现胆囊息肉时首先评估息肉是否为侵袭性或潜在恶性息肉。
4、胆囊息肉病人的总体癌变率随着息肉大小增加而增加,息肉直径<6 mm、6~9 mm和>9 mm的总体癌变率分别为(1.3、8.7、128.0)/10万
5、胆囊息肉直径>15 mm是鉴别肿瘤性息肉癌变的独立危险性。
6、胆囊息肉无蒂与有蒂,无蒂息肉表现为从黏膜层起源的扁平或圆顶状肿块,基底较宽。大多数的恶性或肿瘤性息肉更多表现为无蒂的形态
7、息肉的血管分布研究较少,虽然有研究表明能检测到血管分布的息肉通常为肿瘤性息肉,但并未能说明存在血流信号是恶性肿瘤的独立危险因素,且根据以往经验表明,较大的胆固醇性息肉在彩色多普勒成像中也可能表现出明显的血管分布,因此,共识中认为息肉的血管分布不影响风险分层。
8、大多数胆固醇息肉表现为强回声,但回声可受后方声影、机器参数等影响,评估较为主观。也有研究指出相较于肝脏或者胆囊壁,低回声或等回声的息肉为肿瘤性息肉概率大,但并没有研究表明回声是肿瘤性息肉的独立危险因素[
9、 胆囊壁厚度 ,发现邻近胆囊息肉的局灶性胆囊壁增厚是肿瘤性息肉的显著预测因素
10、胆囊息肉单发及多发 大多研究表明恶性或者肿瘤性息肉中单发比例较多
11、合并结石或胆泥的胆囊息肉恶变率更高
12、息肉的生长与恶变风险,通常认为短期快速生长的息肉恶性可能大。认为息肉直径波动2~3 mm属于息肉自然变化过程。而1年内息肉直径增大至4 mm及以上则构成快速增长,需要进行风险评估。
13、重点:约53%的胆囊癌在初次检出胆囊息肉的6个月内确诊,68%的病人在1年内检出,并且在被确诊的13枚恶性息肉中,9枚为15 mm以上。随访1年后,直径<6 mm的胆囊癌发病率为0,≥6 mm且<10 mm的胆囊癌每年发病率为4.5 /10万,>10 mm者为4.5 /10万。随访第4年后,在最初测量为10 mm或更大的息肉中未发现癌变。因此,共识建议,延长随访时间可能并无更多益处,通常随访3年足以确定绝大多数息肉相关的恶性肿瘤。
14、年龄、合并结石、吸烟、糖尿病、肥胖、绝经前女性肥胖、女性等的胆囊癌患病风险的因素。
15、超声造影 超声造影具有较高的空间和时间分辨率,在息肉定性上比CT和磁共振更具优势。
16、超声造影可优化息肉的可视化特征,且根据强化的时间特征,可鉴别非肿瘤性和肿瘤性息肉以及胆囊癌。非肿瘤性息肉表现为晚期增强,且相较于肝脏呈低增强;而肿瘤性病变表现为明显的早期增强,腺瘤性息肉多表现为偏心性增强或持续均匀增强,恶性息肉则表现为早期强化后逐渐廓清
17、超声内镜相较于常规彩超探头虽能跟接近胆囊以及更适用高频探头,但考虑到超声内镜的有创性,共识指出不建议将超声内镜作为胆囊息肉风险评估的常规检查。
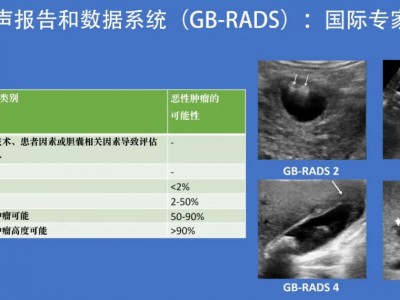
18、胆囊息肉风险评估图
参考文献
(在框内滑动手指即可浏览)
[1] Jørgensen T,Jensen KH.Polyps in the gallbladder. A prevalence study[J].Scand J Gastroenterol,1990,25(3):281-286.
[2] Adsay V,Jang KT,Roa JC,et al.Intracholecystic papillary-tubular neoplasms(ICPN)of the gallbladder(neoplastic polyps, adenomas,and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases[J].Am J Surg Pathol,2012,36(9):1279-1301.
[3] Wennmacker SZ,de Savornin EAJ,Hasami NA,et al.Overtreatment of nonneoplastic gallbladder polyps due to inadequate routine ultrasound assessment[J].Dig Surg,2020,38(1):1-7.
[4] Wennmacker SZ,van Dijk AH,Raessens JHJ,et al.Polyp size of 1 cm is insufficient to discriminate neoplastic and non-neoplastic gallbladder polyps[J].Surg Endosc,2019,33(5):1564-1571.
[5] Szpakowski JL,Tucker LY.Outcomes of gallbladder polyps and their association with gallbladder cancer in a 20-year cohort[J].JAMA network open,2020,3(5):e205143.
[6] Liu K,Lin N,You Y,et al.Risk factors to discriminate neoplastic polypoid lesions of gallbladder: A large-scale case-series study[J].Asian J Surg,2021,44(12):1515-1519.
[7] Washington MK, Goldberg RM,Chang GJ,et al. Diagnosis of digestive system tumours[J]. Int J Cancer,2021,148(5):1040-1050.
[8] He C,Fukumura Y,Toriyama A,et al.Pyloric gland adenoma(PGA)of the gallbladder: A unique and distinct tumor from pgas of the stomach,duodenum,and pancreas[J].Am J Surg Pathol,2018,42(9):1237-1245.
[9] Wiles R,Varadpande M,Muly S,et al.Growth rate and malignant potential of small gallbladder polyps--systematic review of evidence[J].Surgeon,2014,12(4):221-226.
[10] Babu BI,Dennison AR,Garcea G.Management and diagnosis of gallbladder polyps: a systematic review[J].Langenbecks Arch Surg,2015,400(4):455-462.
[11] Rafaelsen SR,Otto PO,Pedersen MRV.Long-term ultrasound follow-up in patients with small gallbladder polyps[J].Dan Med J,2020,67(10):A06200414.
[12] Hertzberg B,Middleton W. Te Gallbladder[M]//Ultrasound Requisites. 3rd ed. Philadelphia,Pa: Elsevier,2015:32-50.
[13] Kubota K,Bandai Y,Noie T,et al.How should polypoid lesions of the gallbladder be treated in the era of laparoscopic cholecystectomy?[J].Surgery,1995,117(5):481-487.
[14] Kim JS,Lee JK,Kim Y,et al.US characteristics for the prediction of neoplasm in gallbladder polyps 10 mm or larger[J].Eur Radiol,2016,26(4):1134-1140.
[15] Choi TW,Kim JH,Park SJ,et al.Risk stratification of gallbladder polyps larger than 10 mm using high-resolution ultrasonography and texture analysis[J].Eur Radiol,2018,28(1):196-205.
[16] Pedersen MRV,Dam C,Rafaelsen SR.Ultrasound follow-up for gallbladder polyps less than 6 mm may not be necessary[J].Dan Med J,2012,59(10):A4503.
[17] Walsh AJ,Bingham DB,Kamaya A.Longitudinal ultrasound assessment of changes in size and number of incidentally detected gallbladder polyps[J].Am J Roentgenol,2022,218(3):472-483.
[18] Buckles DC,Lindor KD,Larusso NF,et al. In primary sclerosing cholangitis, gallbladder polyps are frequently malignant[J].Am J Gastroenterol,2002,97(5):1138-1142.
[19] Fei X,Li N,Zhu L,et al.Value of high frame rate contrast-enhanced ultrasound in distinguishing gallbladder adenoma from cholesterol polyp lesion[J].Eur Radiol,2021,31(9):6717-6725.
[20] Liu XS,Gu LH,Du J,et al. Differential diagnosis of polypoid lesions of the gallbladder using contrast-enhanced sonography[J].J Ultrasound Med,2015,34(6):1061-1069.
[21] Yuan Z,Liu X,Li Q,et al.Is contrast-enhanced ultrasound superior to computed tomography for differential diagnosis of gallbladder polyps? A cross-sectional study[J].Front Oncol,2021,11:657223.
[22] Yuan HX,Cao JY,Kong WT,et al. Contrast-enhanced ultrasound in diagnosis of gallbladder adenoma[J].HBPD INT,2015,14(2):201-207.
[23] Wang X, Zhu JA, Liu YJ,et al. Conventional ultrasound combined with contrast-enhanced ultrasound in differential diagnosis of gallbladder cholesterol and adenomatous polyps(1-2 cm)[J]. J Ultrasound Med,2022,41(3):617-626.
[24] Lin J,Peng X, Dong K,et al. Genomic characterization of co-existing neoplasia and carcinoma lesions reveals distinct evolutionary paths of gallbladder cancer[J]. Nat Commun,2021,12(1):4753.
[25] Castillo J,García P,Roa JC. Genetic alterations in preneoplastic and neoplastic injuries of the gallbladder[J]. Rev Med Chil,2010,138(5):595-604.
[26] Kuipers H, de Bitter TJJ,de Boer MT,et al. Gallbladder cancer: Current insights in genetic alterations and their possible therapeutic implications[J]. Cancers(Basel),2021,13(21):5257.
[27] 赵海鹰,刘金钢.从过度和不足角度看无症状性胆囊结石与胆囊息肉的规范化治疗[J].中国实用外科杂志,2016,36(10):1053-1057.
[28] Wang X, Fu XH,Qian ZL,et al. Non-invasive detection of biliary tract cancer by low-coverage whole genome sequencing from plasma cell-free DNA: A prospective cohort study[J].Transl Oncol,2020,14(1):100908.
[29] 何敏,黄安华,周智辉,等.泡沫细胞形成与胆固醇结石及胆囊息肉形成的相关性研究[J].同济大学学报(医学版),2014,35(3):5-9.
[30] Sung H,Freedman RA,Siegel RL,et al. Risks of subsequent primary cancers among breast cancer survivors according to hormone receptor status[J].Cancer,2021,127(18):3310-3324.
[31] Zheng R,Zhang S,Zeng H,et al. Cancer incidence and mortality in China,2016[J]. JNCC, 2022,2(1):1-9.
[32] 中华医学会外科学分会胆道外科学组,中国医师协会外科医师分会胆道外科医师委员会.胆囊良性疾病外科治疗的专家共识(2021版)[J].中华外科杂志,2022,60(1):4-9.

 微信扫一扫,打赏作者吧~
微信扫一扫,打赏作者吧~